There are models suggesting that the mechanical force from facilitating normal joint movement initiates a cascade of neurophysiological responses from the peripheral and central nervous system affecting the experience of pain. Although, there is a limitation of the current literature and research in the understanding of the biomechanical and neurophysical mechanisms of manual therapy.
Facilitating normal joint movement allows tissue tension and length is returned to normal. The passive range of motion available at a joint depends on how the articular surfaces are able to interact as well as on the surrounding soft tissue’s ability to contract and relax.
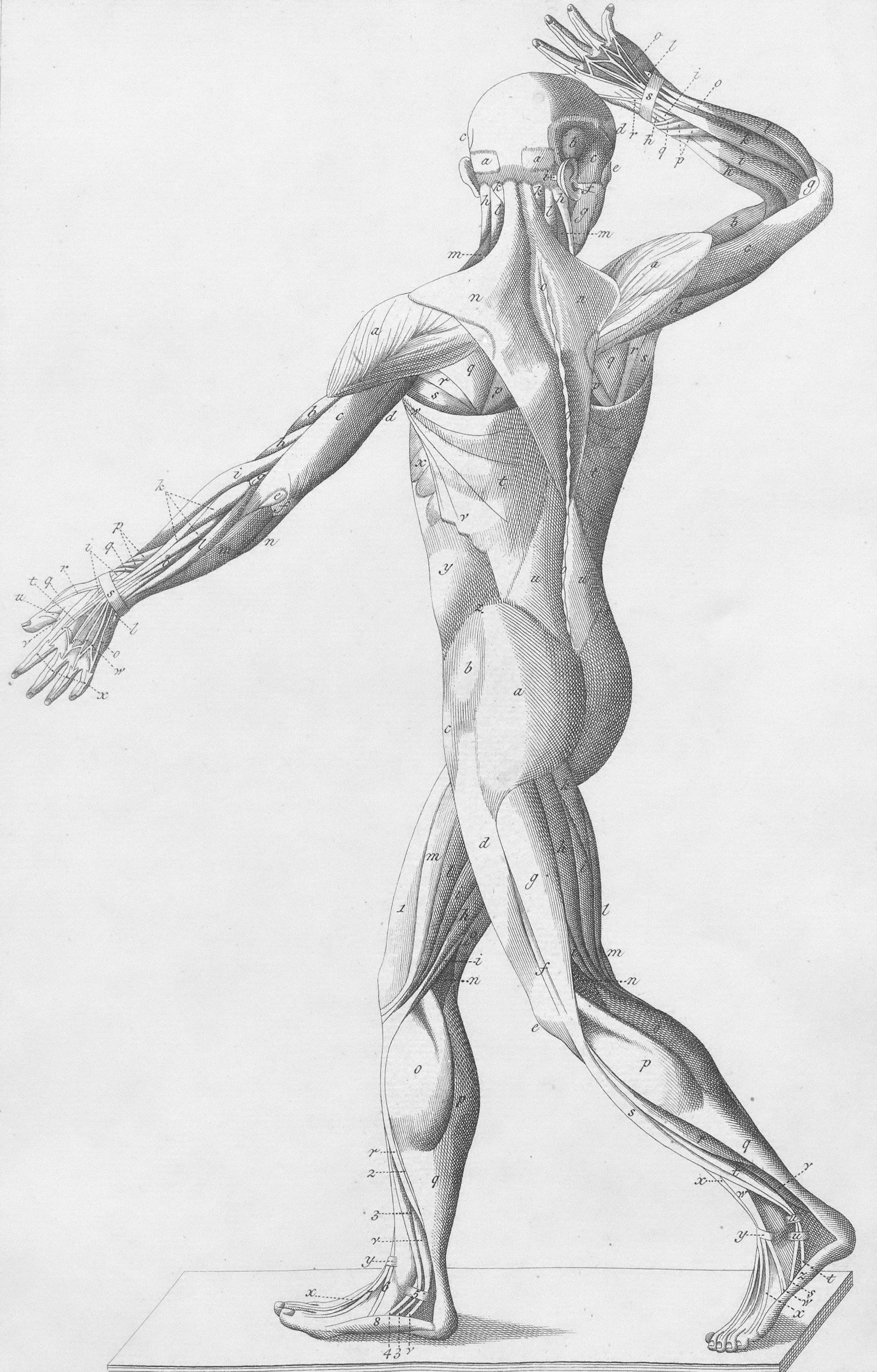
Movement is three dimensional. Therefore, treatment must facilitate all available motions throughout the kinetic chain to assure full recovery. Work in PNF patterns and look for rotational movement. Over fifty percent of motion is in rotation. Pure linear motion where all points move the same distance, does not often occur at joint articulations. Instead, rotational motion is more common, in which there is one point on a bone that remains stationary, and all other points trace arcs of a circle around the point. Flexion and extension cannot exist without rotation. Rotation at the left facet is flexion or extension at the left facet and the same for the right facet.
Find where the patient moves the easiest, where their tissue feels the most relaxed and without tension. A joint’s loose-packed position is located somewhere in its midrange and is the point where the most ligamento-capsular tissue is most relaxed and where movement in any plane is the fullest. Articular receptor activity is also at the lowest in this position.
Supine is the easiest position in which to facilitate joint movement. Each aspect of the joint being prepared for treatment must be supported and protected from unguarded painful movement. Pain produced by unexpected movements of painful joints puts the supporting muscles into spasm and prevents successful treatment. The examiner must be relaxed. The grasp must be firm and protective, but not restrictive.
-
The goal is to facilitate movement at the joint level towards the patient’s neutral posture where the vertebrae are stacked and stable. A neutral head position, when standing, requires 25 Newtons of muscle force to balance the system while a forward head position requires 100 Newton.
Vertebral movement must be facilitated back towards neutral spine position because the vertebrae drop into flexion as gravity is creating a downward force.
The joints will move in the plane of the facet. The goal is to find the loosest position of the joint to allow for the most gentle, precise facilitation of movement. This movement at the joint is accomplished by contralateral rotation and a distraction parallel to the facet joint. Rotation and distraction contralateral at the facet joints translates into extension of the vertebrae towards neutral posture.
Facilitation of movement at the cervical and thoracic vertebra is accomplished with side bend and rotation at the facet joints in the relaxed, supine position. Compression on the thoracic vertebrae in prone with the head rotated to the contralateral side will open up the facets and move them into extension as well. Prone rotation with a posterior-anterior glide and seated rotation are also ways to facilitation movement of the vertebrae closer to the neutral position.
Re-check the tests from the evaluation to assess symmetry right and left. Follow-up with treatment, repeating what you have already done as needed until you are satisfied with the symmetry and outcome.
-
High cervical vertebral movement must be facilitated into extension and neutral posture to allow the TMJ to sit correctly. This will allow the secondary muscle spasm to resolve as well. Once the cervicothoracic region is moving full, then TMJ movement can be assessed directly. TMJ movement can be facilitated to its neutral position with translation and rotation, following the plane of the joint. This is most easily accomplished with the patient supine.
Re-check the evaluative tests you used to determine if TMJ mechanical dysfunction persists. Return to and continue with treatment until the result of these tests are symmetrical.
-
The treatment of the shoulder region begins with the facilitation of joint movement at the cervical and thoracic levels to regain the neutral position. The glenohumeral joint then must be facilitated to its neutral position, if needed, to allow full, functional movement.
Movement at the glenohumeral joint will be most easily facilitated in its loose pack position with the patient supine. The shoulder is passively moved into flexion with a rotational pressure along the joint line.
Re-check with the evaluation tests for symmetry between sides. Continue with treatment until you are satisfied with the outcome.
-
The elbow moves in mainly flexion and extension with rotation occurring at the radio-ulnar joint. You will have the most success facilitating elbow movement with a palmar grip at the ulna just below the joint with a slight valgus pressure. Because the shoulder, elbow and wrist move together, the shoulder and wrist mechanics must also be treated to assure optimal treatment.
Re-check the evaluation tests for symmetry right and left. Continue treatment until you are satisfied with the outcome.
-
Begin by distracting through each metacarpal joint. Line up your forearm with the metacarpal, and with a tight grip, gently pull through the metacarpal joint. Then palpate adjacent carpal bones and rotate through the joint to facilitate normal movement. We are the most stable and therefore the most vulnerable at the third metacarpal which is in line with the capitate and the lunate. Remember that the capitate and lunate bones move opposite of each other. Lunate dislocates ventrally and capitate dislocates dorsally. Walk your fingers through the carpal bones, then visit the radio-ulnar joint and rotate through this joint as well. It will also be important to address mechanical dysfunction at the elbow to assure full wrist movement.
Re-check the evaluation tests and continue treatment until you are satisfied with the symmetry.
-
Begin with PNF diagonals with the patient supine. This is the easiest place to start. Treat both sides. Changing one side changes the other because the pelvis and vertebra are rings. Continue with side lying rotation. Have the patient lay on their side, roll the patient’s shoulder back and the pelvis and lumbar around and up to facilitate movement from the bottom up. Continue with a longitudinal distraction to the right and left legs with a grip at the ankle. This will be a fast movement with the patient supine to distract through the sacroiliac joint and into the lumbar joints.
Then recheck your tests from the evaluation: adduction strength, PSIS level, Baer’s point firmness and tenderness, straight leg raise. Always return to the treatment and then re-check until you are satisfied with the symmetry right and left.
-
Begin central with facilitation of lumbo-sacral joint movement before working specifically at the hip. The hip moves in conjunction with the pelvis and lumbar to create full functional movement. Then continue with facilitation of joint movement at the hip joint specifically if needed. The hip joint will move the easiest in rotation with the patient supine. If there is an arthritic change at the hip joint, then you are able to only resolve the mechanical dysfunction at the lumbar-pelvis and knee. The arthritic change will then be more specific and manageable.
Recheck the evaluation tests, and follow up with treatment until you are satisfied with symmetry right and left.
-
Treatment of the knee should begin with facilitation of joint movement at the lumbo-sacral region, then facilitation movement at the knee. The knee will move into tibial rotation, end range extension, flexion, and recurvatum. It will be easiest to facilitate knee joint movement with the patient resting in supine.
Re-check the evaluation tests and continue with treatment until you are satisfied with the symmetry right and left.
-
An easy place to begin for resolving mechanical joint dysfunction of the ankle/foot is distraction at the metatarsal joints. This is achieved by lining your forearm up with the metatarsal, gripping the toe firmly and gently distracting at the joint line. Follow up with rotational motion between each tarsal joint. And continue with distraction at the subtalar joint. Also visit the fibula-tibia joint and facilitation movement into rotation and an anterior-posterior glide.
Recheck the evaluation tests and continue treatment until you are satisfied with the symmetry right and left.